Infantile Spasms – Primary Steps for Primary Care
A type of severe seizure, infantile spasms require urgent evaluation and treatment. Unfortunately, the diagnosis of infantile spasms is too often delayed because they may be subtle, go unrecognized, or be misdiagnosed as some other less serious condition (i.e., reflux).
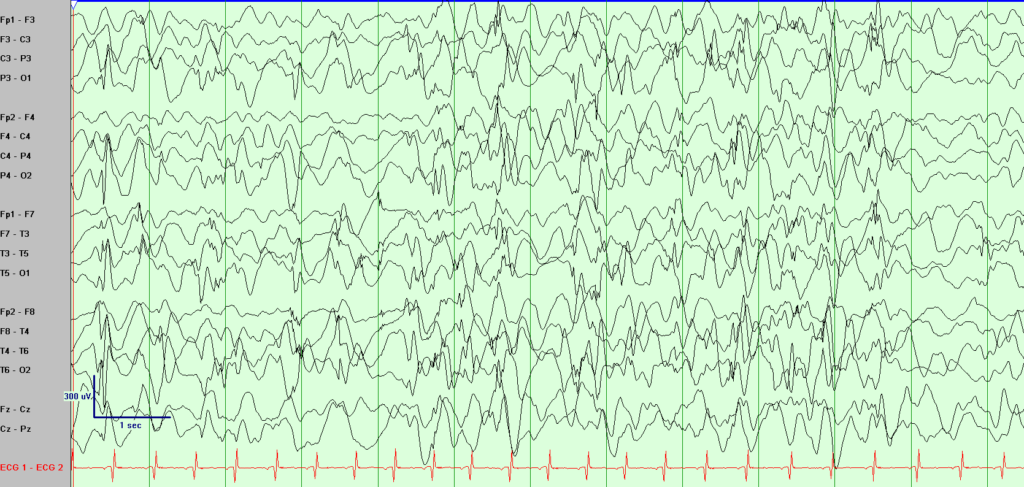
When associated with an electroencephalography (EEG) pattern of hypsarrhythmia (Figure 1), this is known as West syndrome, a severe form of early onset/infantile epilepsy. Infantile spasms are often difficult to control and may cause severe developmental delay, though early treatment with seizure control affords the best opportunity for good developmental outcomes. The majority of children are diagnosed under 12 months of age, with the peak being around 6 months. Children often have associated developmental regression or arrest when the infantile spasms begin; however, some patients may already have developmental delays prior to the onset of this seizure type.
How do you recognize infantile spasms?
This seizure type often presents as a cluster of sudden, repetitive, uncontrolled body movements where the head bobs/nods and the body crunches with the arms extended or flexed. These often occur when the infant is going to sleep or waking up from sleep. While the seizure may initially appear as a startle, the repetitive nature and clustering around sleep are red flags that should not be ignored.
What steps should be taken to evaluate children suspected to have infantile spasms?
It is very helpful if a parent can obtain video of a typical event cluster and review it with their primary care physician/pediatrician.
The next step is urgent and early diagnosis. This occurs through a pediatric neurologist/epileptologist to confirm the diagnosis. Early diagnosis and treatment is imperative to minimize developmental delays.
The diagnosis is confirmed by an electroencephalogram (EEG) and clinical presentation. The EEG usually demonstrates a classic electrographic background called a hypsarrhythmia. This is characterized by a high-amplitude, very disorganized, chaotic brain wave pattern, intermixed with multifocal (differing parts of the brain) spike wave activity (Figure 1). The EEG during the seizure is often characterized by a high-voltage slow wave, followed by electodecrement (i.e., flattening of the EEG).
If infantile spasms are recognized early enough, the pattern may not yet be present, but this should not delay the diagnosis. If the clinical presentation is consistent with infantile spasms, appropriate treatment should be started regardless of the EEG findings.
What causes infantile spasms?
There are multiple reasons children develop infantile spasms and the underlying etiologies will vary. Common causes are abnormalities of the brain which may be congenital (i.e., the brain is malformed prior to birth) or acquired (i.e., injury occurs later such as stroke, brain infection, etc.). Other reasons include genetic/metabolic causes, though in many cases the cause remains unknown.
What treatment options are available for infantile spasms?
Standard first line treatment in the United States is high-dose steroids, such as prednisolone or adrenocorticotropic hormone (ACTH) or vigabatrin. Both medications are approved for first line treatment for infantile spasms. Vigabatrin is often used first line if the etiology of infantile spasms is tuberous sclerosis complex (TSC). Treatment protocols for steroids differ with both high-dose, short duration and low-dose, long duration treatments commonly used. Studies are ongoing to determine if there are better approaches to therapy, such as combination therapy or treatment to prevent spasms (particularly for patients with TSC).
What should you do if you suspect infantile spasms?
The Jane and John Justin Neurosciences Center at Cook Children's is available to evaluate children suspected to have infantile spasms urgently – typically within days. Please call 682-885-2500 for urgent infantile spasms referrals.
Research at Cook Children's for infantile spasms
Cook Children's is a longstanding member of the Pediatric Epilepsy Research Consortium (PERC), a multi-center collaboration of U.S. pediatric epilepsy centers dedicated to improving care of children with epilepsy. Cook Children's participated in the Early Onset Epilepsy Project, which enrolled patients with new onset epilepsy (ages 28 days to 36 months) to identify predictors and outcomes in early life epilepsies, including the diagnosis of new onset infantile spasms. To date, a total of 775 children were recruited from 17 centers. As a result of this collaboration, multiple manuscripts highlighting diagnosis, treatment, etiologies and outcomes have been published.
Studies of note:
Response to treatment in a prospective national infantile spasms cohort. Knupp K, et al. Ann Neurol, 2016. This manuscript looked at response rates of treatment and showed first-line standard therapies (i.e., ACTH or vigabatrin) should be used as initial treatment for infantile spasms, regardless of the underlying etiology, including those with impaired development or known structural or genetic/metabolic etiology.
How should children with West syndrome be efficiently and accurately investigated? Results from the National Infantile Spams Consortium. Wirrell, E, et al. Epilepsia, 2015. This study demonstrated that genetic testing, specifically genetic testing such as chromosomal microarray and epilepsy gene panel, are high yield. For patients enrolled in this PERC study, these two tests yielded a definitive diagnosis in >40% of patients presenting with new onset spasms without an obvious cause after initial clinical evaluation and MRI.
The impact of hypsarrhythmia on infantile spasms treatment response: Observational cohort study from the National Infantile Spasms Consortium. Demarest S, et al. Epilepsia, 2017. This study demonstrated first-line therapy (prednisolone, ACTH, vigabatrin) should be considered as standard treatment even if the typical EEG pattern of hypsarrhythmia is not present in a patient with a diagnosis of infantile spasms. First-line treatment with standard therapy was shown to be the most important variable in determining likelihood of response to treatment of infantile spasms with or without hypsarrhythmia.
Immediate outcomes in early life epilepsy: A contemporary account. Berg A, et al. Epilepsy & Behavior. 2019. This PERC study demonstrated epilepsy within the first year of life (regardless of etiology) should always be viewed as of utmost urgency and importance until proven otherwise. This article highlights predictive risk factors for patients with early life epilepsies including infantile spasms. It discusses the risks for children including drug resistance, developmental delay and developmental worsening after diagnosis.