Technology: 3T Intraoperative MRI – Better imaging for better care
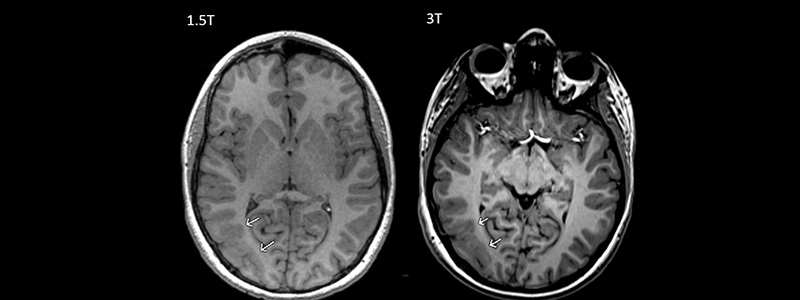
MRI images reveal the structure and functional processes of the body to an extent unparalleled by CT scan and other radiographic techniques without exposing patients to ionizing radiation. Hydrogen atoms in our tissues, when subjected to a high-frequency magnetic field, can be induced to generate radio-frequency signals detectable by antennas placed close to the skull. Varying the radio signal can “tune in” for different tissues, depending on their hydrogen atom structural array and produces the images radiologists review. The resulting anatomic images are astonishing on 1.5-Tesla magnets, but doubling magnet strength from 1.5- to 3-T improves image quality even more (Figure). In 2017, Cook Children's upgraded our intraoperative MRI (iMRI) to 3-T strength to improve the quality of images obtained during surgery. iMRI allows the child to be scanned in the operating room before completion of the procedure, thus the surgeon can review images and return to perform additional surgery if needed before completing the case.
Epilepsy
The utilization of 3-T imaging should have several benefits over the prior 1.5-T system. 3-T MRI's sensitivity increases the identification of structural brain lesions responsible for focal-onset epilepsy which could lead to better identification and complete resection of epileptogenic lesions. For example, in a retrospective review on 50 sets of MR images of 25 patients undergoing both 3-T and 1.5-T brain imaging with a dedicated epilepsy protocol, 3-T outperformed 1.5-T, being over twice as likely to identify and characterize structural brain lesions1 including cortical dysplasia, an important cause of focal-onset epilepsy in children. 3T's heightened susceptibility effects may increase the detection of previously “cryptic” cavernous malformation hemorrhage, another source of epileptogenesis. Even treatment of nonlesional epilepsy benefits from 3-T, as definition of cortical and vascular structures improves accuracy of stereo EEG electrode placement, minimizing the likelihood of injury to superficial and deep blood vessels. Finally, laser ablation, which uses light energy to destroy epileptogenic tissue, relies upon accurate intraoperative imaging data. Introducing the resolution of 3-T into laser ablation not only facilitates target identification, but also yields more precise delineation of damage volume during and after ablation thanks to much keener diffusion weighted imaging.
Brain tumors
Complete brain tumor resection (as opposed to incomplete tumor removal) is associated with superior outcome for virtually every child harboring a primary brain tumor, therefore the goal of brain tumor resection should be, with few exceptions, total resection. Since 2007, we have been employing intraoperative MRI during brain tumor surgery to increase the safety and extent of tumor resection. 3-T's superior views of the operative area permits very aggressive, yet safer, tumor resection and should help to perform more complete surgery the first time avoiding the need for repeat procedures.
Functional neurosurgery
3-T can also benefit children undergoing DBS (deep brain stimulation) for the treatment of movement disorders, a procedure necessitating “on the fly” electrode trajectory adjustments. 3-T iMRI allows co-registration of preoperative planning images (always 3-T) with the real-time images, allowing faultless electrode placement with accuracy well under 1mm.
We are grateful to the Jane and John Justin Foundation who have allowed us to introduce 3T imaging into the operating room suite, continuing the intraoperative imaging program brought to life by the “Refuse to Lose” campaign.