Innovation: Cutting-edge Imaging to Improve Pediatric Stroke Care
The incidence of pediatric stroke is steadily increasing, with most recent rates up to 13 per 100,000 children per year – similar to that of childhood brain tumors. Stroke is one of the leading causes of death in children, and 20 percent of children who have had a stroke will have a recurrence.
The Cook Children's Comprehensive Stroke and Thrombosis Program, one of 16 such centers in the U.S., is led by Fernando Acosta Jr., M.D. (Neurology) and Marcela Torres, M.D. (Hematology) with additional support from neurosurgery, neuro-radiology, neuropsychology, a dedicated nurse practitioner, nurse, social worker and Child Life specialist. The team is committed to the early recognition, treatment and prevention of pediatric stroke through research, innovation and education. As members of the International Pediatric Stroke Society, the Cook Children's team works with a network of other pediatric hospitals to improve stroke care worldwide.
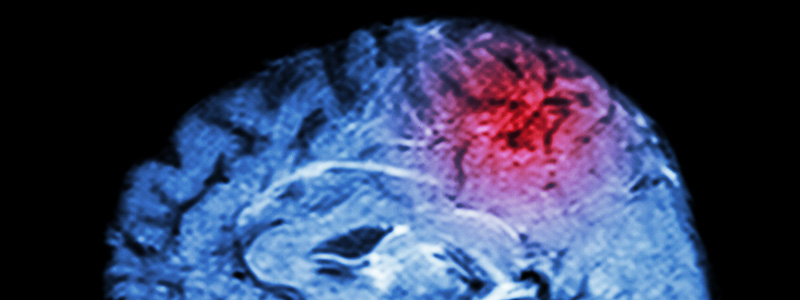
Cook Children's has recently employed the use of novel imaging techniques to guide therapy and interventions aimed at reducing the risk of future strokes. Intracranial vessel wall MRI (case study, figure 1) is an innovative diagnostic imaging technique that allows evaluation of intracranial vascular pathology by directly visualizing arterial vessel wall abnormalities with MR sequences. With this technique, it is possible to identify distinct pathologic findings within the intracranial vessel wall itself, ranging from arterial dissection to vasculitis. Understanding the pathology then allows the team to select therapy specific to the etiology, which is expected to improve outcome.
The team also utilizes perfusion weighted imaging, which consists of a variety of MRI techniques that give insight into the perfusion of the brain tissue by the blood. This imaging technique provides critical information regarding the mean transit time (time it takes blood to reach specific areas of the brain), cerebral blood volume (amount of blood reaching specific areas of the brain) and cerebral blood flow (constant amount of blood reaching specific areas of the brain). These factors can be used to predict areas in the brain that are at risk for injury or subsequent stroke. Through these advanced imaging techniques, the Cook Children's Comprehensive Stroke and Thrombosis Program aims to continue improving the recognition, treatment and outcome of pediatric stroke.
Case Study:
A 3-year-old with sudden onset of left side body and face weakness was transferred from an outside hospital to Cook Children's intensive care unit. A magnetic resonance image (MRI) and magnetic resonance angiography (MRA) of the brain and neck showed extensive infarct of the right hemisphere in a watershed distribution, along with narrowing of the right carotid artery with multifocal narrowing of other intracranial arteries. While a typical MRA was completed (Figure 1a), vessel wall imaging (Figure 1b) more clearly demonstrated the inflammatory changes in the vessel wall from vasculitis which resulted in the child's stroke. The patient was treated with anticoagulation and steroid therapy based on these findings. Follow-up scans (Figure 1c) show resolution of vessel wall inflammation.

Case study, figure 1
Pediatric Stroke and Thrombosis Program
Dr. Fernando Acosta (Neurology)
Dr. Marcela Torres (Hematology)
Time is critical.
If you suspect your patient has had an acute stroke, call Cook Children's Teddy Bear Transport at 1-800-543-4878. The Cook Children's Pediatric Stroke and Thrombosis Program also accepts referrals for children with a history of stroke. Call 682-885-8050 for more information.